CRC patients with these clinical characteristics need more frequent post-op chest imaging
New research supports the development of standardized imaging surveillance protocols for patients who have been diagnosed with colorectal cancer.
The research was presented at the Scientific Forum of the American College of Surgeons (ACS) Clinical Congress 2022. In the study, experts highlighted some of the clinical characteristics of patients who are most likely to develop lung metastases, suggesting patients with these increased risks would benefit from more frequent chest imaging after their diagnosis and treatment.
“With this study, we sought to develop a strategy that is evidence-based to determine how frequently, at what intervals, and for how long patients at risk of developing lung metastases should undergo imaging of their chest,” study co-author Mara Antonoff, MD, FACS, associate professor, thoracic and cardiovascular surgery, UT MD Anderson Cancer Center said in a news release.
The experts noted that up to 50% of colorectal cancer patients develop metastases, with cancer spreading to lungs in around 18% of cases. Patients who go on to develop lung metastases would benefit from early detection and, in some cases, surgery, the experts pointed out.
For the study, researchers reviewed the cases of 1,600 patients with colorectal cancer. Of these, 14.6% developed lung metastases at a median of 15.4 months following colorectal surgery.
The experts found increased risks of cancer spread in patients with a need for systemic therapy at the time of their colorectal cancer surgery, higher lymph node ratios and KRAS mutation.
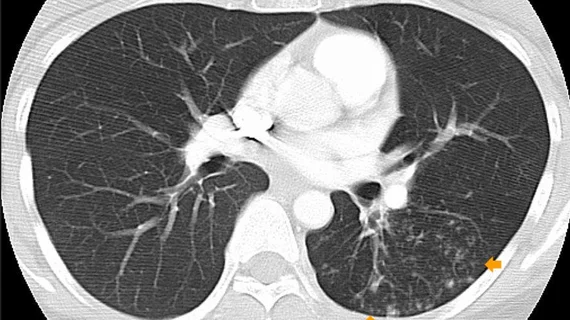
These patients were at the greatest risk of developing lung metastases within three months of surgery, prompting the researchers to recommend that they undergo frequent chest CT or PET imaging.
Lead author Nathaniel Deboever, MD, a general surgery resident at UTHealth Houston McGovern Medical School and co-authors noted that, although the characteristics make sense from a clinical perspective, they bring greater light to the need for standardized surveillance in certain groups of patients.
“A concrete clinical application of this research, following validation, is to build evidence-based guidelines affecting chest surveillance in patients with resected colorectal cancer,” Deboever said in a statement. “These guidelines will hopefully allow high-risk patients to undergo radiographic screening in a timely manner, permitting the early diagnosis of pulmonary disease.”
The research team next hopes to validate their work in a separate group of patients to formalize imaging and surveillance protocols.
To learn more, click here.