New data highlight inconsistencies in imaging protocols for pediatric appendicitis
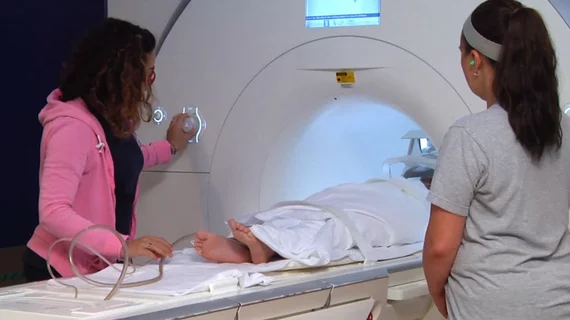
Utilization of MRI for instances of suspected appendicitis in the pediatric population is beneficial, yet its deployment varies across institutions. Consequently, this has resulted in a lack of standardized protocols when appendicitis is in question.
These and other findings were published recently in the American Journal of Roentgenology. Experts surveyed 100 members of the Society of Chiefs of Radiology at Children’s Hospital (SCORCH) to better understand how MRI is utilized for suspected appendicitis across a pediatric population, and they found a mixed bag of results [1].
Of the 39 SCORCH members who completed the survey, a little over half (21/39) reported that their institution performs MRI for acute appendicitis when patients present to the ED. Just four of those institutions use MRI as first-line imaging, with most of the others (18/21) opting for ultrasound first, followed by MRI.
MRI is available 24/7 at 15 out of those 21 facilities. In instances when MRI is not immediately available, some patients are instructed to wait until it becomes available, and others undergo CT instead.
Protocols for ruling out acute appendicitis also vary, according to the data. Though experts involved in this latest work maintain that there is an ideal protocol, there are no set standards.
“The optimal MRI protocol for acute appendicitis should be rapid and accurate,” explained corresponding author of the paper Rama S. Ayyala MD, with the Department of Radiology at Cincinnati Children's Hospital Medical Center. “Short protocols facilitate patient throughput and cooperation.”
The majority of respondents indicated that their institution uses protocols that extend from the upper abdomen to the lower pelvis, but the consistency of the responses ended with that. The number of reported sequences ranged from three to eight; 12 unique sequences were reported, with an axial T2-weighted sequence without fat saturation being the only one included in every facility’s protocol.
Scan times ranged from 8 to 30 minutes, and room times ranged from 20 to 30 minutes. Contrast use was not common.
The authors suggest that standardization of rapid protocols could reduce scan times and improve patient care. They acknowledge that their findings are limited to pediatric hospitals and might not accurately depict patterns at other institutions.
To learn more, click here.