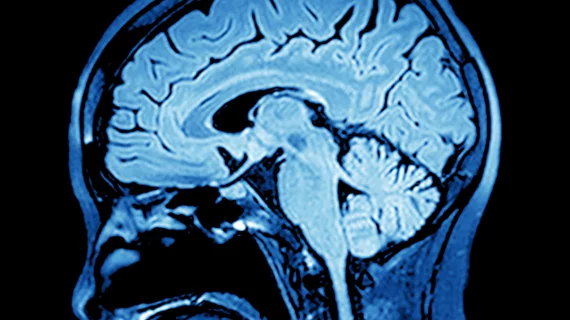
Advanced MRI shows potential for assessing asymptomatic patients at risk for Alzheimer’s
Cognitively normal people with a genetic mutation associated with Alzheimer’s disease show lower white matter integrity on brain imaging compared to those without the gene, suggesting MRI may be a useful weapon in the battle against the disease.
That’s according to a five-year exploratory analysis comparing structural brain connectivity differences among patients, published Tuesday in Radiology.
MetroHealth Medical Center researchers in Cleveland previously discovered that patients with sporadic AD—about 99% of cases—gradually show white matter structural connectivity degradation as amyloid accumulates. This investigation builds on that finding, with diffusion tensor MRI demonstrating similar results among at-risk patients without symptoms of memory loss.
“This shows the potential of MRI as an evaluation tool in patients who are deemed at risk for Alzheimer’s disease before they develop symptoms,” lead author Jeffrey W. Prescott, MD, PhD, a neuroradiologist at MetroHealth, said in a statement. “Use of these advanced MRI techniques could help further refine identification of at-risk patients and risk measurements.”
The findings are based on data from the Dominantly Inherited Alzheimer Network and involved 30 mutation carriers (mean age 34) and 38 non-carriers (mean age 37). All participants showed no memory issues when undergoing imaging.
Those exam results showed people with the autosomal-dominant Alzheimer disease (ADAD) mutation had lower structural connectivity in areas connecting the brain’s parietal and frontal lobes, both regions involved with AD. And among mutation carriers, Prescott et al. also found a correlation between expected years until symptoms arose and white matter connectivity.
The researchers say their study supports using imaging brain markers in people with genetic risk factors associated with early Alzheimer’s.
“One potential clinical use of this study tool would be to add quantitative information to risk factors like family history and use that to help identify patients early, when they may benefit from treatment,” Prescott added. “But until we have an effective treatment, we will have to wait for that to be implemented.”