Stroke care still lags among certain Medicare populations
As access to stroke imaging increases, so too does the likelihood that a patient can utilize lifesaving interventions, but experts are concerned about a multitude of disparities that inhibit populations from receiving such care.
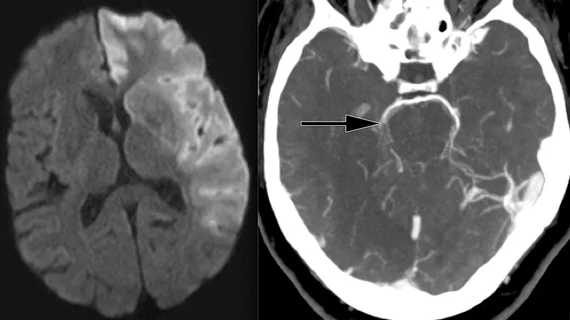
A new study published in the Journal of the American College of Radiology found significant increases over the last decade in the use of computed tomography angiography (CTA), computed tomography perfusion (CTP) and MRI for the Medicare ischemic stroke population in areas where access to neuroimaging was readily available. Patients in these areas were also more likely to undergo procedures such as endovascular thrombectomy (EVT) and intravenous thrombolysis (IVT), both of which positively impact mortality rates.
However, healthcare disparities remain prevalent among certain demographic groups within the Medicare population, the experts found. Despite increases of 250% for CTA and 428% for CTP, researchers observed lower rates of neuroimaging utilization among rural residents, older individuals (80 years and above), women and Black patients.
“Understanding recent trends and socioeconomic disparities in neuroimaging utilization among patients with ischemic stroke, and how imaging relates to clinical treatment decisions and outcomes, is critically important for clinicians and health care policymakers as we strive to ensure optimal and equitable access to high-quality stroke care across an increasingly diverse and aging population,” corresponding author Jason J. Wang, PhD, from the Department of Radiology at the Donald and Barbara Zucker School of Medicine at Hofstra/Northwell in Hempstead, New York, and co-authors explained.
The analysis of 85,547 ischemic stroke patients found that between 2012 and 2019, access to CTA, MRA and MRI scans decreased patient mortality rates, while CTP was associated with higher mortality rates post discharge. Utilization of neuroimaging increased markedly from 2012 to 2019. Though these increases were seen throughout the United States, numbers in rural and southern areas, such as “the Stroke Belt,” continued to lag behind urban areas. Access to imaging was found to be related to method of treatment as well.
“Disparities existed in neuroimaging utilization across all demographic groups,” the authors wrote. “Given these associations, understanding the root causes of the observed disparities is paramount to achieving equity in stroke care across the population.”
Related neuroimaging content:
New MRI technique helps physicians ID multiple sclerosis lesions
CMS coverage decision for Alzheimer's drug, related PET scans sparks concern in imaging community
Memory complaints associated with structural brain abnormalities and increased dementia risk
Better neuroimaging guidelines could save practices millions, research shows
MRI findings associated with poor thrombectomy outcomes after stroke