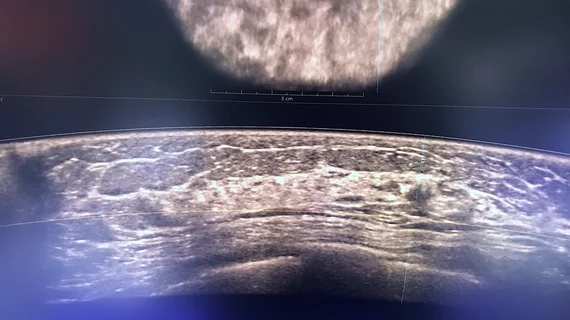
Automated ultrasound excels for women with dense breasts
Automated breast ultrasound has numerous advantages over mammography, especially for women with dense breasts, according to new data.
Experts recently compared the use of automated breast ultrasound (ABUS) to other screening strategies to assess how the modality performs in terms of cancer detection rates, false positive biopsy rates, sensitivity and specificity. After analyzing the cases of more than 19,000 women, experts concluded that an ABUS and screening mammogram combination yielded better overall performances than mammography alone and mammography in conjunction with handheld ultrasound (HHUS).
In comparison to mammography alone, the strategy that included ABUS and mammography was particularly beneficial for detecting cancer in women aged 45-54 years with dense breasts. Experts involved in the study highlighted the importance of this finding, as both mammography and HHUS have drawbacks that inhibit their performance in instances of increased breast density.
“As a newly introduced imaging technology, automated breast ultrasound (ABUS) has an increased reproducibility compared with HHUS due to the separation of image acquisition and interpretation process,” corresponding author of the new Academic Radiology paper Fanghui Zhao, MD, PhD, with the Chinese Academy of Medical Sciences and Peking Union Medical College, and co-authors explained.
Prior to this research, there has been limited data on how ABUS compares to HHUS and mammography in asymptomatic women. The team used the data of 19,171 women from six hospitals in China to compare the modalities. Asian women have higher rates of increased breast density and are more often diagnosed with breast cancer at younger ages than women of other races, the group explained, adding that there is a great need to determine the most effective screening strategies among the Asian population.
The group compared three strategies—mammography alone, mammography and ABUS, and mammography and HHUS. Detection rates were higher when ABUS and HHUS were utilized in comparison to mammography alone, notably so in women with dense breasts, the experts reported. Compared to HHUS, the use of ABUS was also found to improve false positive biopsy rates, as its use identified specific image features that distinguish between malignant and benign tumors.
“The standardized review process allows ABUS to be viewed as a potential solution for reducing the high variation among operators using HHUS,” the group suggested. “Another advantage is that it can be automatically reconstructed to 3D views and allow interpretation in the addition plane (coronal), providing more information to help detect lesions.”
The authors suggested that although ABUS has the “potential to be a replacement tool for HHUS,” more research is needed on the feasibility and cost-effectiveness of this strategy.
The study abstract can be viewed in Academic Radiology.