Younger women with breast arterial calcifications are at markedly higher risk of major cardiovascular events
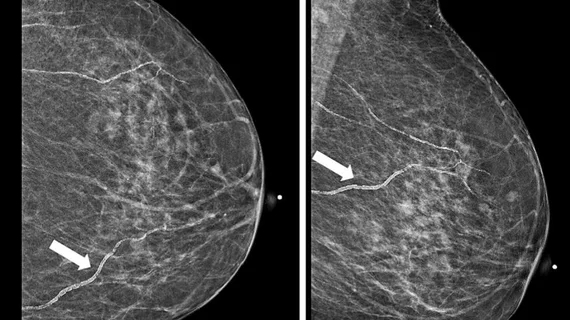
Numerous studies have linked the presence of breast arterial calcifications (BACs) on mammograms to increased risk of cardiovascular disease. Now, new research is prompting calls for BACs not just to be included in radiology reports, but for their presence to be quantified as well.
Published in the Journal of the American College of Cardiology, the study details the accuracy of an artificial intelligence quantification tool that analyzes BACs to predict risk of major cardiovascular events and mortality. The study found that women with higher AI-automated BAC scores were nearly three times as likely to die from cardiovascular-related complications, such as acute myocardial infarction, heart failure and stroke.
“It is postulated that BAC represents lifetime exposure to risk factors related to arterial stiffening, which increases the risk of CVD through both coronary and noncoronary mechanisms (i.e., heart failure and stroke),” corresponding author Tara Shrout Allen MD, with the Division of Preventive Medicine at the University of California-San Diego, and co-authors explained. “However, routine clinical use of BAC has not been adopted due to a lack of outcomes studies as well as technological challenges in measuring and reporting BAC.”
Researchers sought to determine whether further elaborating on the presence of BACs would provide more detailed insight into women’s CVD risk. To do this, they applied an AI quantification tool to nearly 20,000 screening mammograms.
The algorithm identified regions with a high probability of BACs and then used imaging features, like density, contrast and other physical dimensions, from those areas to quantify the presence and severity of BACs. The images were given a score, which incorporated both presence and quantity, from 0-100, with higher scores signaling greater BAC severity.
BACs were present in around 23% of the exams. After a median follow-up of six years, death occurred in 7.8% of women with BACs and 2.3% of those without. Just over 12% of women with BACs experienced a heart attack, stroke or were diagnosed with heart failure, while this occurred in just 4.3% of women without the finding.
The risk of mortality significantly rose with each 10-point increase in BAC score. The finding was “especially predictive” of future CVD-related events when identified in younger women, most notably in those ages 40 to 59.
“Results from this study and others suggest that BAC may develop at an earlier age than other traditional cardiovascular risk factors, and thus could serve as an early biomarker of underlying ASCVD risk,” the group noted. “These findings are important since they suggest that early risk stratification with BAC in younger women may help identify new candidates for lifestyle modification and preventative therapies and may ultimately help improve their outcomes.”
Prior research has indicated that although the majority of radiologists are aware of the association between BAC and CVD, just 15% include them in mammography reports. Currently, there is no standardized reporting requirement related to BACs, and the American College of Radiology classifies reporting vascular calcifications on breast imaging as optional.
One concern related to standardizing BAC reporting is its resultant impact on radiologists’ workflows. The group suggested that AI quantification tools similar to the one used in their research could help ensure that workflows are not disrupted and encourage greater buy-in from radiologists.