New scoring system for 'second look' breast lesions could decrease biopsies by 30% or more
A new scoring system for “second look” breast lesions detected on MRI scans could reduce breast biopsies by up to 30%, according to newly published data in Clinical Radiology.
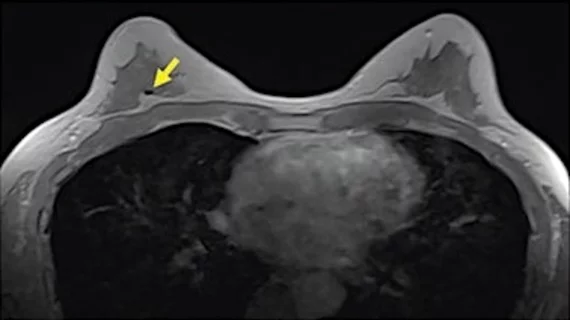
These second look lesions are findings that were not identified on initial mammogram or ultrasound exams; they are typically classified using the American College of Radiology’s BI-RADS lexicon, but experts involved in the new study noted that the final lesion category assigned is still vulnerable to subjectivity. To address this, a team from University Hospitals of Leicester NHS Trust in the United Kingdom recently developed a new system to fulfill the need for an objective and reproducible way to differentiate between malignant and benign second look breast lesions on MRI for women with known breast cancer.
“This is unique in that the population assessed has an increased risk of additional malignancy than the general population without known malignancy, and so, in general, the threshold for biopsy or further study may be lowered for these patients," corresponding author K. Ziada and colleagues explained. "However, recall of all 'second-look' lesions for further assessment or sampling leads to increased patient anxiety, undue workload, and even over-treatment,”
The team collected data on 95 second-look lesions from their facility over a period of two years to identify features indicative of malignancy based on confirmed histopathological analyses. Lesions were assessed according to margins, T2 signal, internal enhancement patterns, contrast kinetics and diffusion-weighted imaging patterns.
Out of 95 lesions, 52% were found to be malignant. The most common contrast kinetics for these lesions was the plateau pattern followed by the washout pattern, while the progressive pattern was typically observed in benign lesions. Additionally, an apparent diffusion coefficient cutoff value of 1.1 was found to be best for differentiating between benign and malignant lesions.
A score of 2 or more points as a marker of who should be referred for biopsy based on the above features was observed to be 100% accurate. If the system had been initially used on the lesions included in the study, it would have helped to decrease biopsies by 30%, the experts noted.
The team suggested that this system has high reliability for clinical use and can spare many patients from invasive biopsy without the risk of missing malignancy.
The study abstract is available here.