PET quantification method can help improve amyloid pathology assessment
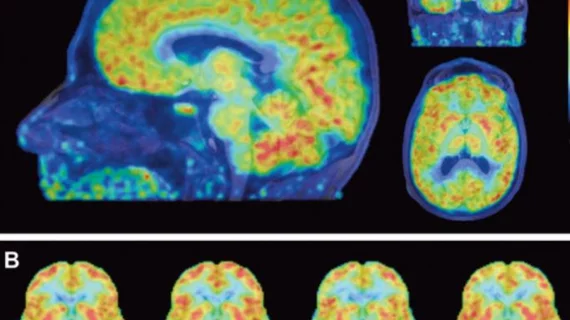
Utilizing non-displaceable binding potential (BPND) quantification with 18F-Flutemetamol PET imaging can better assess amyloid pathology in elderly patients with low amyloid buildup compared to traditional standard uptake value ratio (SUVr), reported authors of an Oct. 12 study in the Journal of Nuclear Medicine.
Currently, identifying amyloid burden through summed late images or via semi-quantitative SUVr imaging is considered “sufficient,” wrote corresponding author Lyduine E. Collij, with VU University Medical Center in The Netherlands, and colleagues.
“It has been shown, however, that SUVr overestimates amyloid burden compared with quantitative BPND,” Collij et al. added. “As such, quantitative BPND images may be more reliable also for visual interpretation.”
With this in mind, Collij and researchers included dynamic 18F-Flutemetamol PET scans from 190 cognitively normal elderly patients with a mean age of 70.4 years in their study, of which 185 were included.
Three trained readers blinded to clinical information analyzed all SUVr images and all BPND images. Results showed, “moderate” (.57) inter-reader agreement in the visual assessment of SUVr, and “good” (.77) agreement for BPND images, according to authors. For the entirety of cases, the mean ±SD values for SUVr and BPND were 1.33 (± 0.21) and 0.16 (± 0.12), respectively.
Additionally, there was disagreement between readers in 35 SUVr cases and 15 cases with BPND images. Ninety-one percent of SUVr discordant cases were classified as negative based on semi-quantitative measurements, the authors noted.
“In a cognitively normal elderly population with low amyloid burden we show a considerable improvement in inter-reader agreement of 18F-Flutemetamol visual assessment when using BPND rather than standard SUVr images,” the authors wrote. Additionally, they added that “misclassifications can be reduced using semi-quantitative SUVr measures and avoided using fully quantitative BPND measures.”
Collij and colleagues argued their results could help avoid false-positive classification in early population drug-intervention studies and research examining cerebral blood flow change in correlation to age and disease progression.