MRI improves liver fat monitoring in obese patients
For obese patients who undergo weight loss treatments, a specialized MRI sequence may provide a safe and noninvasive way to monitor liver fat levels and the success of treatments, according to new research published online Dec. 18 in Radiology.
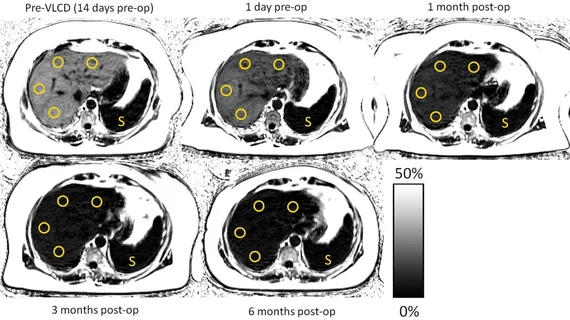
Researchers assessed liver fat levels before and after bariatric surgery though quantitative chemical shift encoded MRI (CSE-MRI), a noninvasive imaging technique that measures proton density fat fraction (PDFF) as a biomarker of liver fat concentration. The technique ultimately provides liver fat as a percentage to help physicians better monitor changes over time.
“In addition to demonstrating the clinical utility and feasibility that CSE-MRI provides in the monitoring of hepatic PDFF over time, our analysis provided a number of insights into reductions in liver fat content following bariatric surgery,” wrote lead author Dustin Pooler, MD, radiology fellow at the University of Wisconsin School of Medicine and Public Health in Madison, and colleagues.
It’s estimated that more than two-thirds of American adults are clinically overweight or obese. For these patients, non-alcoholic fatty liver disease is common and can progress to cirrhosis or increase their risk of liver cancer.
Bariatric surgical procedures have proven to be effective weight loss interventions but the problem, as Pooler and colleagues explained, is the lack of research exploring the connection between bariatric surgery, weight loss and decreases in liver fat content.
Moreover, “a barrier to understanding these relationships has been the lack of reproducible, noninvasive methods to quantify liver fat,” the researchers wrote.
From June 27, 2010 through May 5, 2015, Pooler and colleagues enrolled 50 patients—including 43 women (average age 50.8 years) and seven men (average age 51.7 years)—with severe obesity who had undergone bariatric surgery for weight loss. They also went on a low-calorie diet (600 to 900 calories per day) before the surgery.
The participants underwent preoperative CSE-MRI exams two to three weeks before surgery to determine their PDFF for liver fat concentration. A second MRI scan was performed one to three days before surgery, with the participants’ BMI, weight and waist circumference recorded during both examinations.
SE-MRI scans were conducted at one month, three months and six to 10 months after surgery to measure changes in PDFF. Measurements of BMI, weight and waist circumference were taken again at each interval.
The researchers found a notable decrease in the participants’ average PDFF six to 10 months after surgery. Average PDFF decreased from 18 percent to five percent—five percent is within normal limits.
Additionally, the average estimated time for PDFF levels to normalize was roughly five months. The initial PDFF was also the only strong predictor of both liver fat loss and time to normalization, according to the researchers.
"The results showed a rapid early phase of improvements in liver fat, followed by a phase of continued improvements at a slower pace," Pooler said in a prepared statement. "The changes began with the initiation of the low-calorie diet and occurred in advance of the overall improvements in BMI among the patients."
Overall, the results point to several ways CSE-MRI may be used in the management of obese patients with fatty livers regardless of starting anthropometrics or degree of weight loss following surgery.
“Consequently, it may be reasonable to consider the severity of hepatic steatosis—independent of weight or BMI—when deciding to enroll a patient for bariatric surgery,” the researchers wrote. “Furthermore, if liver PDFF is of interest to the clinician, it may be reasonable to follow PDFF with CSE MRI in addition to or instead of other anthropometric measurements.”