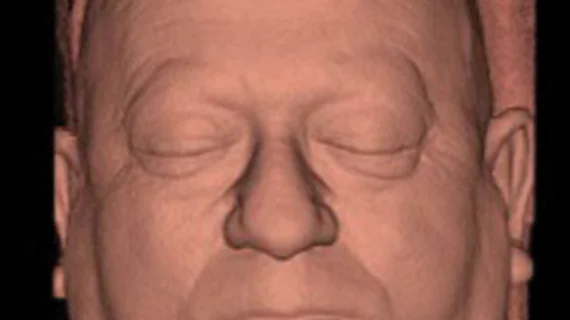
Algorithm classifies sleep apnea—or recognizes its absence—from 3D headshots
A predictive algorithm has distinguished patients free of obstructive sleep apnea (OSA) from those with three levels of the condition—mild, moderate and severe—with 91% accuracy. And it did so using only 3D photos of the subjects’ faces.
The study behind the achievement was conducted at the University of Western Australia and published in the Journal of Clinical Sleep Medicine.
Peter Eastwood, PhD, and colleagues took 3D headshots of 400 individuals—100 in each of the four categories above.
To ascertain the facial topography most predictive of the presence and severity of OSA, the team used the (unprinted) 3D photos to measure linear and geodesic distances between points and along angles. Geodesic distances are the shortest lines between points over a curved surface.
Using a subset of the image data to train a supervised machine learning algorithm, the researchers used linear discriminant and receiver operating characteristic analyses to assess the accuracy of different measurement combinations.
Upon repeating these analyses using different thresholds of the Apnea Hypopnea Index (AHI), the team found that, relative to linear measurements, the geodesic measurements improved the ability to identify individuals with and without OSA (86% for linear vs. 89% for geodesic).
They also found the best classification performance, 91% accuracy, came when they combined linear and geodesic measurements into a single predictive algorithm.
“This study suggests that 3D photographs of the face have predictive value for OSA and that geodesic measurements enhance this capacity,” authors conclude.
In an accompanying open-access article, Ofer Jacobowitz, MD, PhD, of Icahn School of Medicine in New York City and Stuart MacKay, MD, of the University of Wollongong in Australia comment that the work by Eastwood and colleagues presents sleep medicine with a new challenge: how to incorporate such research into clinical practice.
“While image-analysis technology appears to be easy to implement and inexpensive, it is based on a correlation with the AHI, an imperfect metric for OSA,” they write.
Still, the study at hand “provides a modern, innovative addition to the diagnostic assessment of patients for OSA,” Jacobowitz and MacKay comment. “It is hoped that photographic image analysis can be merged with other, easily obtained parameters from patient history, soft tissue examination, and physiological endo-typing to direct improved and individualized treatment for our patients.”
In a news release sent by the American Academy of Sleep Medicine, Eastwood points out that obstructive sleep apnea is “a huge public health problem, and despite effective treatments being available, many with OSA are currently undiagnosed. Therefore, simple, accurate screening tools are needed to predict those who have OSA.”