Obesity and Alzheimer's look similar on brain imaging, cause comparable neurodegeneration
New MRI research suggests that obesity and Alzheimer’s disease (AD) affect the brain in similar ways.
According to the study, published in the Journal of Alzheimer’s Disease Jan. 31, these findings offer evidence supporting the notion that obesity contributes to cognitive decline comparable to that of AD because it causes similar neurodegeneration. Specifically, experts found that both obesity and AD can result in excess grey matter cortical thinning.
“Our study strengthens previous literature pointing to obesity as a significant factor in AD by showing that cortical thinning might be one of the potential risk mechanisms,” explained the study’s first author Filip Morys, a PhD researcher at The Neuro (Montreal Neurological Institute-Hospital) of McGill University.
For the study, researchers analyzed the brain MRIs of 1,300 individuals from the UK Biobank and the Alzheimer’s Disease Neuroimaging Initiative (ADNI). Scans of participants with AD were compared to those of healthy controls and the imaging of obese individuals was analyzed alongside scans of leaner individuals.
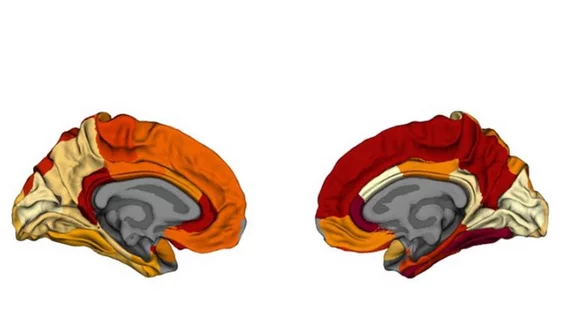
Experts used imaging from each group to create maps of grey matter atrophy. Those maps were also compared to available amyloid-β/tau protein maps.
Experts found that the obesity maps were very similar to the AD maps. Specifically, they observed thinning in the right temporo-parietal cortex and left prefrontal cortex on both maps. No correlations were identified between the obesity maps and the protein maps.
These findings suggest that obesity does, in fact, contribute to greater neurodegeneration similar to that which is observed in patients with AD, and that it could also play a role in the development or severity of AD.
The good news? These risks can be addressed with interventions directed toward weight management, the authors concluded.
“Excess weight management could lead to improved health outcomes, slow down cognitive decline in aging, and lower the risk for AD.”
The study can be viewed here.