Higher radiation doses don't always improve CT image quality
When it comes to CT exams, higher radiation doses do not always equate to better image quality.
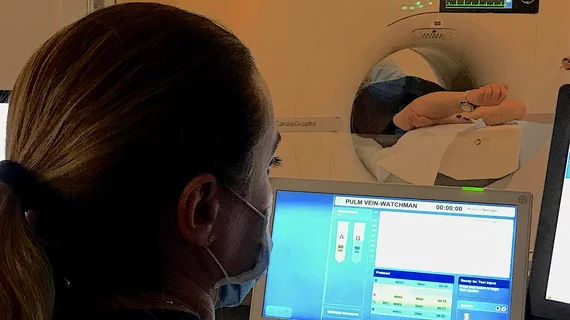
Keeping patients’ cumulative radiation exposure as low as possible while also obtaining high quality exams has long been the primary goal of radiation safety initiatives and equipment manufacturers alike. In recent years, manufacturers have developed numerous dose reduction methods, many of which utilize artificial intelligence to improve image quality.
However, with so many legacy systems still in place, dose reduction protocols, whether they include AI assistance or not, vary across scanners and organizations. This can create inconsistencies in both image quality and measuring patients’ total radiation exposure.
A new paper in the European Journal of Radiology examines how such variances in radiation dose reduction methods vary across scanners, vendors and imaging departments, in addition to how these methods affect overall image quality.
“Due to differences in both hardware and software solutions between vendors and across scanners, standardization of image quality and radiation doses across scanner generations and vendors is increasingly challenging,” corresponding author Anne Catrine T. Martinsen, with the Department of Life Sciences and Health at Oslo Metropolitan University in Norway, and co-authors explained. “Different practices within radiology departments significantly influence the outcomes of image quality and dosimetry, as they are affected by local solutions and set-ups.”
For the analysis, researchers scanned an anthropomorphic phantom once with local abdominal CT protocols on 40 CT scanners, from four vendors, in 33 sites. Three experienced radiologists quantitatively evaluated image quality of liver and kidney parenchyma based on contrast-to-noise ratio (CNR) and signal-to-noise ratio (SNR), before recording the volumetric CT dose index (CTDI VOL) for each scan.
The team noted variances in CNR across all scanners, even when the doses used were the same. Older scanners were found to have 12% lower CNR despite having 15% higher CTDI VOL. In assessing doses and image quality, the team did not observe a significant relationship between CTDI VOL and CNR.
Overall, the agreement between radiologists was acceptable for all dose and image quality groups, other than those with the highest CNR.
“The correlation between image quality and radiation doses was weak, indicating that higher doses do not consistently improve CNR,” the group noted. “These findings emphasize the importance of considering both dose and image quality in the future establishment of diagnostic reference levels.”
The group suggested that their findings highlight a need for more refined image quality criteria for abdominal CT to optimize dose reduction efforts across vendors in the future.
“The study results are useful as a benchmark in image quality and radiation dose optimization efforts. In addition, other anatomical regions could benefit from benchmarking similar to the current study.”
The abstract is available here.