Imaging data backs physical activity as guard against Alzheimer’s
Increasing daily physical activity may help older adults delay their progression to Alzheimer’s disease (AD), according to research published July 16 in JAMA Neurology.
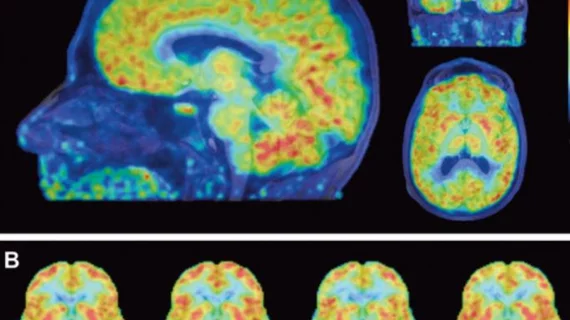
Upon analysis of 182 individuals, PET and MRI scans showed that older patients who were more physically active had less beta-amyloid accumulation and gray matter volume loss, even after adjusting for vascular risk, according to Jennifer S. Rabin, PhD, with Massachusetts General Hospital (MGH), and colleagues.
“Our findings are consistent with a rich literature suggesting that greater engagement in physical activity is associated with a lower risk for dementia due to AD,” Rabin, with MGH’s Department of Psychiatry, and colleagues added. “Importantly, these associations remained significant after adjusting for vascular risk, supporting the view that the protective effect of physical activity on cognitive decline and neurodegeneration does not solely occur via mechanisms related to vascular risk.”
Boosting daily physical activity has gained traction as a possible strategy to maintain brain health and cognition in older adults, the authors explained. Animal and human studies alike have found more physical activity can preserve cortical gray matter structure and slow β-amyloid (Aβ) accumulation and tau burden, but most of this research has not assessed Aβ burden.
Rabin and colleagues set out to study if baseline physical activity is protective against Aβ-related cognitive decline and neurodegeneration in 182 clinically normal adults who were part of the Harvard Aging Brain Study (HABS). Baseline activity was quantified in mean steps per day, and all participants had prior baseline Aβ PET data, baseline medical data for vascular risk and longitudinal neuropsychological and structural MRI data.
The results showed that greater physical activity was associated with slower Aβ-related cognitive decline (β coefficient 0.03; P < .001) and gray matter volume loss (β, 482.07; P = .002). Vascular risk did not change these associations, the authors noted, and was independently associated with slower Aβ-related decline (Aβ, −0.04; P < .001) and volume loss (β, −483.41 P = .01).
“…these findings support interventions that target both physical activity and management of vascular risk factors as a means of delaying cognitive decline and neurodegeneration in preclinical AD,” the researchers wrote. “These lifestyle interventions could be coupled with anti-Aβ or anti-tau treatments when they become available.”