'Visual hindsight bias': What it is and how it affects lawsuits against radiologists
"Hindsight bias” is a psychological phenomenon describing the notion that people believe they can make better predictions or decisions once they have been exposed to new information on the subject, often causing them to overestimate their own abilities.
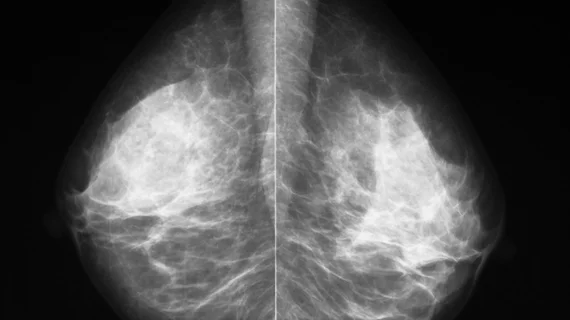
Radiologists are especially susceptible to what is referred to as “visual hindsight bias” that can make them feel as though having prior knowledge about an image can improve their perception of it. Due to their increased vulnerability to visual hindsight bias, radiologists who specialize in interpreting mammograms are more likely to be sued for a missed finding in comparison to their peers.
A new paper in the Journal of Medical Imaging explores how such a phenomenon impacts breast radiologists to better understand whether these biases are visual or cognitive, in addition to how visual hindsight bias might impact litigation against such specialists.
“Evidence suggests it is not only a decision-making phenomenon but also a visual perception one, where prior information about an image enhances our visual perception of the contents of that image,” corresponding author of the new paper Hayden M. Schill, with the University of California San Diego, and colleagues explained. “The current experiment investigates to what extent expert radiologists perceive mammograms with visual abnormalities differently when they know what the abnormality is (a visual hindsight bias), above and beyond being biased at a decision level.”
The team included 34 radiologists in their analysis. Each radiologist was presented with a series of mammogram images with abnormalities. Using the “repeated imaging with single evaluation” or the “RISE” method, the team presented the images to readers in an unpredictable order, with some seeing noisier images toward the beginning of the series, followed by clearer images and vice versa. Readers were asked to note whether the abnormalities correlated with a mass or a calcification in addition to sharing their level of confidence in their decision.
This method ensures that any noted biases are strictly visual, not cognitive.
The team found that radiologists who were presented with clearer images first were more likely to make more accurate, confident diagnoses when they were later given blurry images to read. This finding is in line with their hypothesis, supporting the notion that gaining prior information from a clear image better informs readers when presented with the same image with increased noise—a solid example of visual hindsight bias in practice. Their findings also suggest that there are some cases where no radiologist can identify certain lesions at first glance, which could have implications in a courtroom.
“This paper suggests that the phenomenon of 'missed' lesions on a previous mammogram subsequently found 'in hindsight' by another radiologist after diagnosis is an effect of the visual hindsight bias and not only a decision-level error,” explained Professor Maryellen L. Giger, PhD, editor-in-chief of the Journal of Medical Imaging. “The results of this paper have implications for not only negligence lawsuits against radiologists but also the general population of patients who wonder ‘what if the lesion had been found earlier?’”
The team suggested that future work should focus on finding strategies to mitigate hindsight bias in radiology, as these could also have implications for malpractice or negligence lawsuits.
The detailed study is available here.