Shear-wave elastography predicts fetal growth issues earlier than standard of care
Values derived from ultrasound shear-wave elastography exams of the placenta could offer important insight into fetal growth restrictions.
A new analysis in Clinical Imaging details placental shear-wave elastography findings that differ between pregnancies with normal and abnormal fetal growth rates. Specifically, experts found that placental elasticity differed significantly between the two—a finding that could have important implications for determining fetal growth restrictions (FGR) much earlier in pregnancies.
“Fetal growth restriction presents a significant challenge in prenatal medicine, affecting approximately 5%–20 % of pregnancies. FGR is associated with a higher rate of adverse perinatal outcomes, such as preterm and still births, increased risk of fetal distress during labor and early neonatal deaths,” corresponding author Zareen Fatima, with the Faculty of Allied Health Sciences at the University of Lahore in Pakistan, and colleagues explained. “The ability to accurately diagnose and monitor FGR is of paramount importance for timely clinical intervention and the optimization of fetal outcomes.”
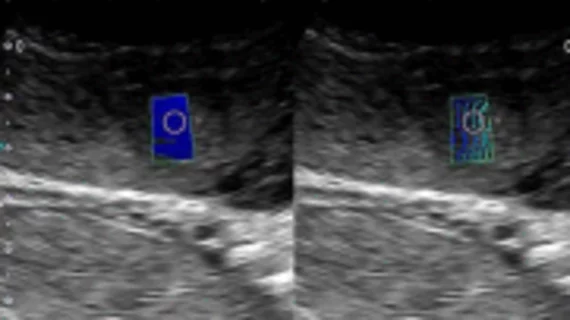
Currently, obstetric ultrasound with fetal biometry measurements and Doppler imaging is routinely used to identify FGR. However, in recent years, shear-wave elastography has emerged as an option that can provide greater detail into tissue health.
“Ultrasound elastography offers the potential to detect alterations in the placental tissue associated with FGR earlier and more accurately than conventional ultrasound parameters alone,” the authors suggested.
To determine the effectiveness of the technique, the team conducted standard obstetric ultrasound plus shear-wave elastography imaging on a group of 121 pregnant women, 54 of whom showed normal fetal growth and 67 with FGR. Restricted growth was defined as the fetal weight below the 10th percentile for gestational age.
Placental elasticity differed significantly between the two groups, specifically in the measurements of PE (kilopascals, kPa) and shear wave speed (meters per second, m/s). The authors suggested that these findings support prior research indicating that FGR is the result of placental dysfunction, which is owed to altered biomechanical function and can be ably detected through shear-wave elastography.
“These results from direct mechanical testing and sonoelastography are reinforced by evidence from many studies that FGR is associated with extensive histological architectural alterations, including increased syncitiotrophoblastic apoptosis, fibrosis, thickening of trophoblastic epithelium, reduction in elastin with an increase in collagen component, decidual vascular atherosis, and infarcts etc.,” the group explained. “These changes impair placental function and metabolism.”
The team noted that their exams were conducted across the placenta without distinguishing between the central (near umbilical cord insertion) and peripheral portions, while at least one previous study focused on specific regions. Two of those studies (Sugitani et al. and Altunkeser et al.) highlighted higher elasticity values in the central region, near the point of cord insertion. The group suggested that measurements taken in that region could be more reproducible and serve as a starting point for standardizing shear-wave elastography exams of the placenta.
“It essentially provides us as an identifiable and anatomically fixed point especially in cases of central cord insertion,” the authors explained.
Although the study had limitations, the team maintained their findings support the notion that shear-wave elastography can accurately identify and predict the severity of FGR earlier than the current standard of care in terms of imaging.
Learn more about the study’s findings here.